There is a new procedure that could restore male fertility by reimplanting frozen testicular tissue in order to obtain sperm for fertility treatments
New Procedure Offers Hope for Restoring Male Fertility through Reimplantation of Frozen Testicular Tissue

There is exciting news in the field of fertility treatments as researchers have developed a groundbreaking procedure that shows promise in restoring male fertility. This new approach involves reimplanting frozen testicular tissue to obtain sperm for fertility treatments, providing hope for couples struggling to conceive.
According to a recent article published in the New Scientist, this procedure aims to address male infertility caused by a variety of factors, such as genetic disorders, chemotherapy, or radiation treatments. Traditionally, when sperm cannot be retrieved directly from the testes, couples have had limited options, such as sperm donation or adoption. This new procedure offers an alternative solution that could revolutionize male fertility treatments.
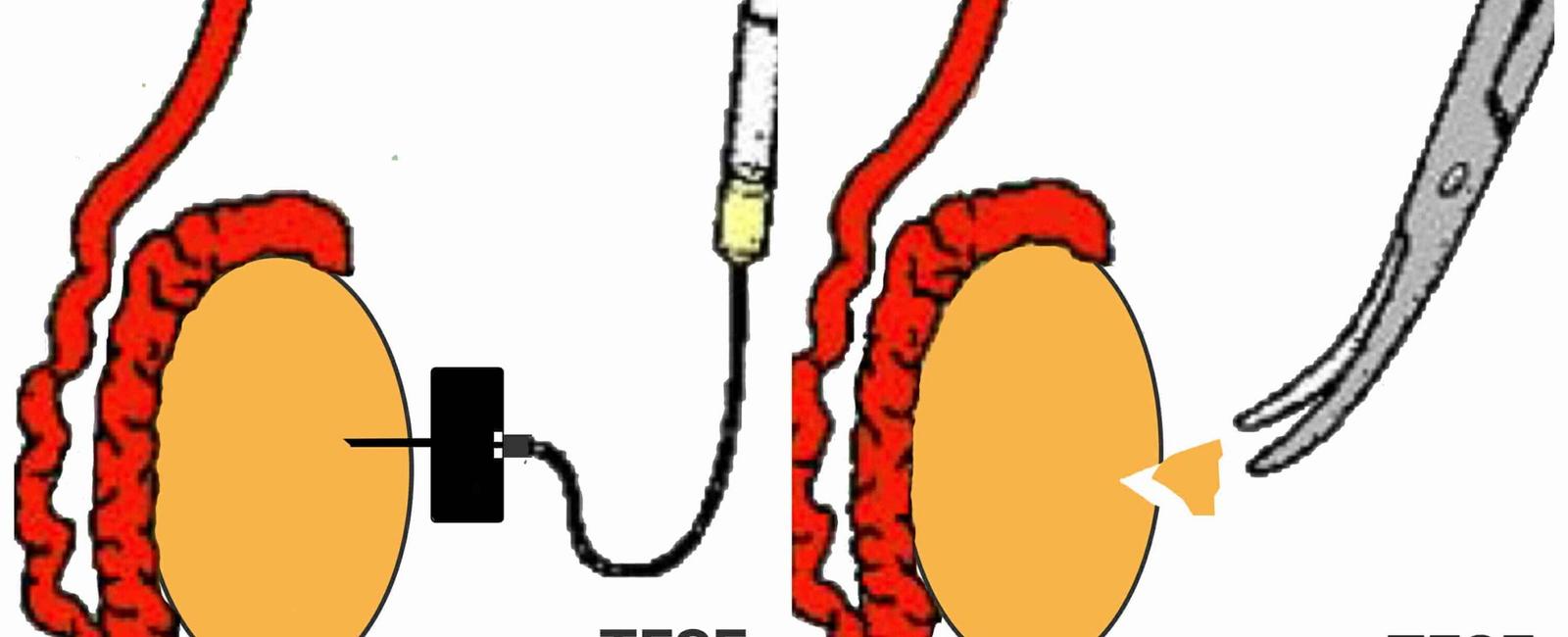
The process begins by extracting testicular tissue from the male partner and freezing it for preservation. This is done before any treatment that may harm fertility, such as cancer therapies. Once the individual is ready to start a family, the frozen tissue is thawed and reimplanted back into the testes. Over time, the tissue begins to produce sperm, which can then be retrieved for assisted reproductive techniques, such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
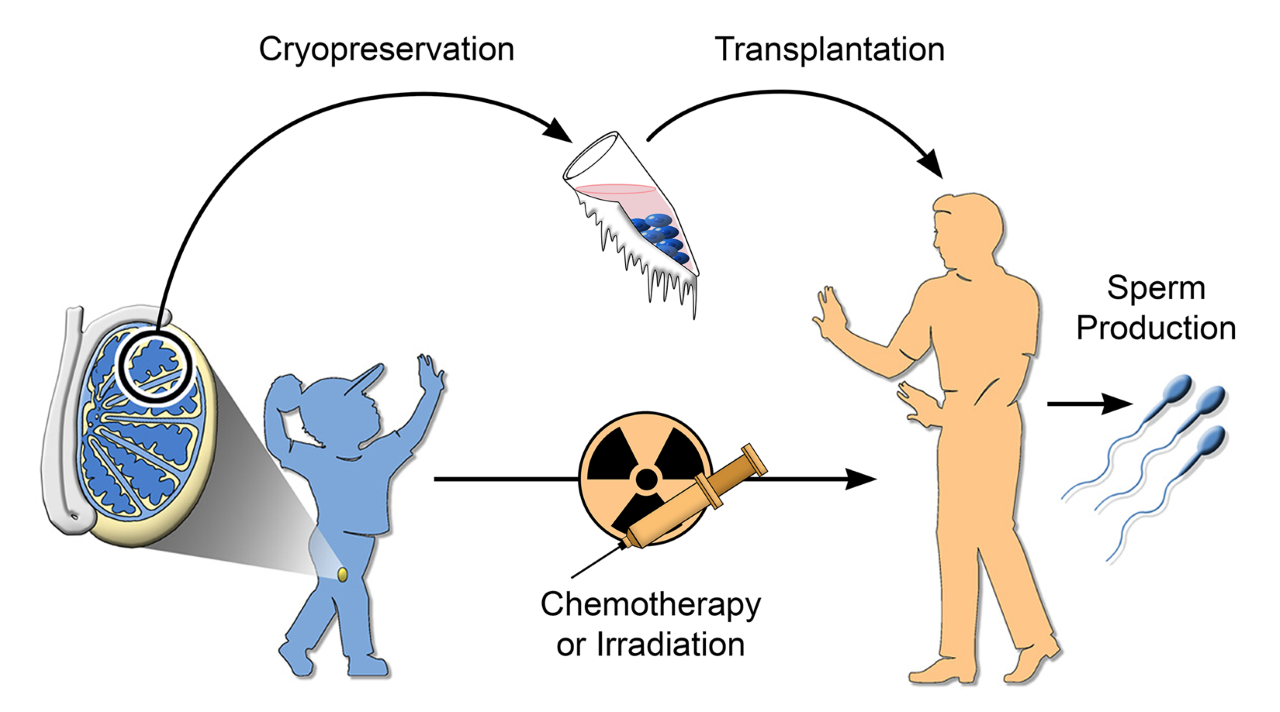
This innovative procedure offers several advantages over other existing methods. Firstly, it allows individuals to preserve their fertility before undergoing treatments that may compromise it. This is especially crucial for those diagnosed with conditions that require aggressive therapies such as chemotherapy or radiation. By preserving testicular tissue, patients can have hope for future parenthood once they have overcome their health challenges.
Secondly, using reimplanted testicular tissue to obtain sperm reduces the emotional burden often associated with using a sperm donor. Couples can have biological children together, strengthening the bond within their family unit. This breakthrough paves the way for a more inclusive and personalized approach to fertility treatments.
While this procedure is still in the experimental stage and requires further research and refinement, the preliminary results are promising. Scientists have successfully restored fertility in animals using this method, providing hope for its application in humans. However, it is essential to exercise caution and remain realistic about the potential outcomes until further studies are conducted.
To stay updated on the latest advancements in male fertility restoration, it is advisable to refer to reliable sources like the New Scientist article “Male fertility could be restored by re-implanting frozen testes tissue.” This informative piece discusses the research behind the procedure, highlights its potential benefits, and provides insights into its future implications.
In conclusion, the development of a new procedure that involves reimplanting frozen testicular tissue offers hope for restoring male fertility. This groundbreaking approach has the potential to revolutionize fertility treatments, providing individuals with a chance to conceive biologically regardless of their previous health challenges. While further research is needed, the initial results are encouraging, and scientists remain optimistic about the future of male fertility restoration.
Share
Related Posts
Quick Links
Legal Stuff